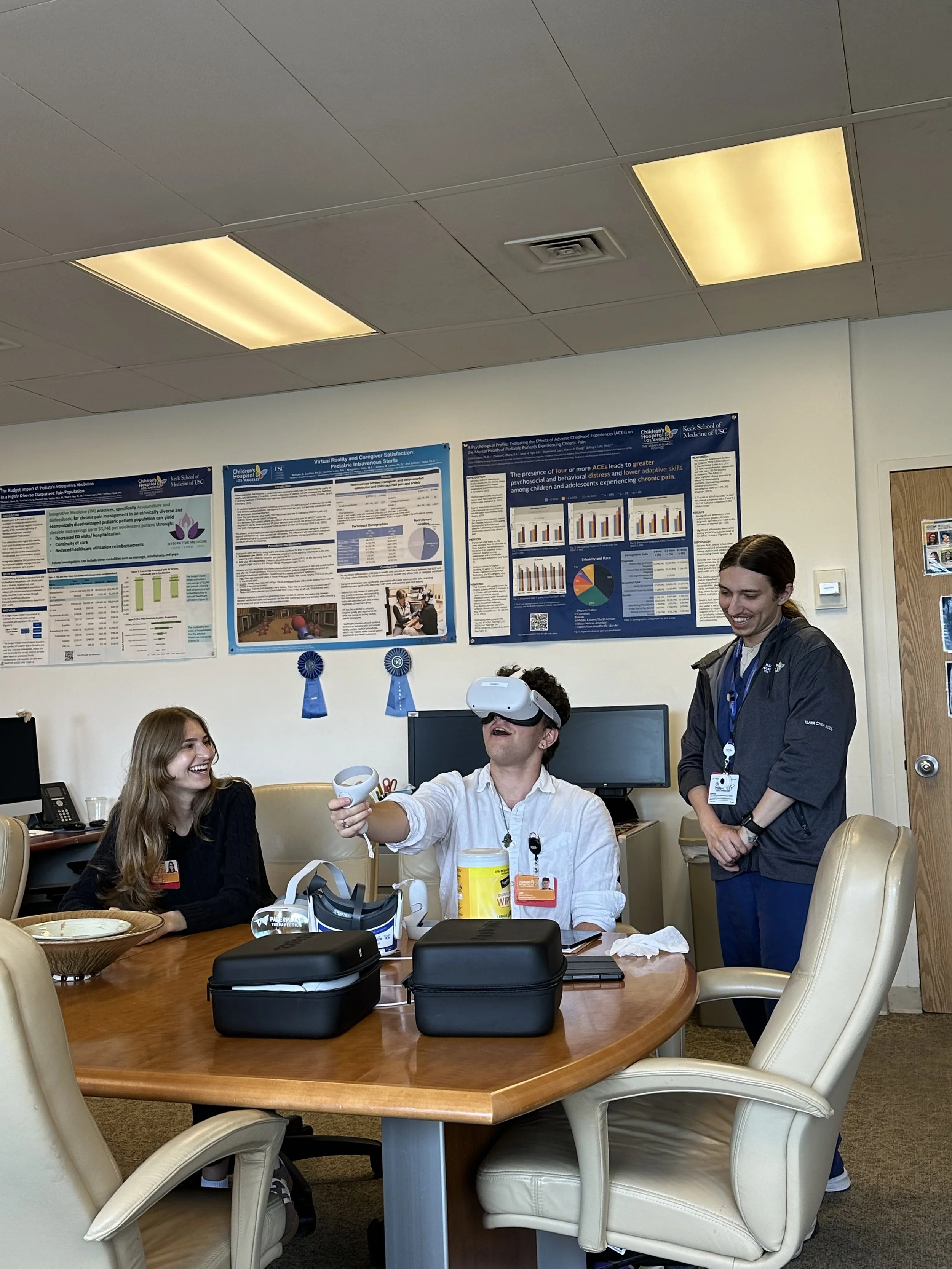
Virtual Reality
Virtual Reality to Reduce Pain and Anxiety During Painful Procedures
Background | Distraction is a form of non-pharmacological intervention for reducing pain and anxiety in children during painful medical procedures (e.g., venipuncture, IV placement). Recent technological developments in the area of virtual reality (VR) provide new and potentially more effective ways of distracting children from the pain and anxiety associated with medical procedures. While initial studies of VR pain distraction are promising, few have studied the effectiveness of the technology in children, using a multi-method approach.
Study | The current study aims to recruit 240 children ages 7-21 and their caregivers who arrive at the hospital for an outpatient painful medical procedure. Children and their parents will be randomly assigned to one of two treatment conditions: 1) existing hospital standard of care or 2) standard of care plus distraction via VR. Children and caregivers will be asked to complete measures assessing pain and anxiety both before and after the procedure. In addition, objective measures of child pain and distress during the medical procedure will be taken using coding of behavioral/verbal expressions.
Objectives | 1) To determine if VR is more effective than standard care for reducing pain and anxiety in children undergoing painful medical procedures. 2) To evaluate caregiver’s assessment patient distress and satisfaction with VR compared to standard of care for patients undergoing painful medical procedures. 3) To evaluate healthcare provider's assessment of patient cooperation and their satisfaction with VR compared to standard of care.
Inclusion/Exclusion Criteria | Inclusion: English-speaking CHLA patients between ages 7 to 21 undergoing a painful medical procedure. Patients must be in the normal range of development. Exclusion: Patients will be excluded if they: 1) are currently taking pain or anxiolytic medication, 2) have a psychiatric disorder, organic brain syndrome, intellectual disability, or other known cognitive/neurological disorders, 3) have visual, auditory, or tactile deficits that would interfere with the ability to complete the experimental tasks, 4) have a history of seizure disorder, 5) are experiencing flu-like symptoms, headache, or earache, or 5) have known or suspected motion sickness.
Funding | Funded by AppliedVR LLC.
Preliminary Qualitative Findings
“Great way to do procedure without anesthesia.”
— Patient Parent
“So grateful to CHLA for offering. All hospitals should.”
— Patient Parent
Effect of Virtual Reality on MRI Preparedness
Background | Magnetic resonance imaging is an important and increasingly prevalent imaging modality used in healthcare. Children often find the procedure anxiety provoking causing difficulty in staying still and providing quality images. The use of preparation techniques including play therapy and role play utilizing such tools as a fiberglass mock MRI have shown to reduce anxiety and facilitate better image quality. Modalities of preparation including Virtual Reality (VR) pose as an alternative to habituate children for a MRI procedure.
Study | Experimental group participants will be exposed to an educational virtual reality mock MRI training titled “Ready Teddy”. This training explains the procedure to the viewer and addresses common questions that individuals often have regarding an MRI. Furthermore, using audio/visual cues, when the viewer moves their head too much in a MRI like setting they are reminded to stay still. Biofeedback training is aimed to mimic the experience of the MRI with real audio recordings of image acquisition, in order to adequately train the view to stay still in an MRI procedure. These activities will be carried out by research staff. Control group participants will receive the standard of care which includes a discussion of the procedure with the patient and their family administered by a Child Life Professional or member of the clinical team.
Objectives | 1) Preparation for a MRI with a virtual reality MRI simulation will reduce participant and parent anxiety. Aim 2) Use of Virtual Reality MRI simulation will result in less motion during a MRI.
Inclusion/Exclusion Criteria | Inclusion: Patients between the ages of 8-10 years scheduled for a clinical MRI at CHLA. Exclusion: Patients will be excluded if they: 1) have metal in their bodies, 2) have a medical history that may affect brain development and require sedation for an MRI, 3) have epilepsy or a history of seizures, 4) have a history of MRI acquisition where habituation and preparedness may not be needed, 5) speak English as a second language, or 6) have implantable medical devices or personal medical devices that may be affected by the study device’s radio waves.
Funding | Funded by Lumeum Inc.